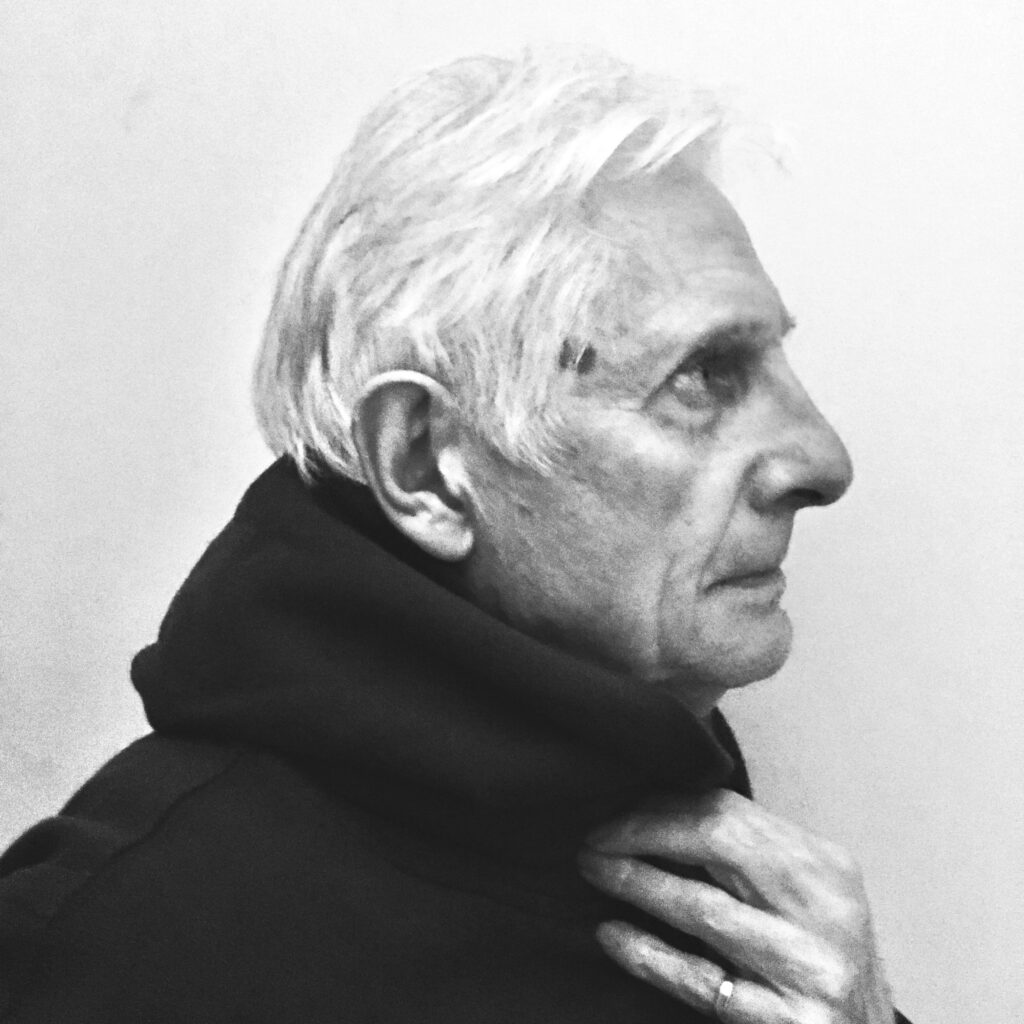
M.M.
BY BERT STERN
LONGING TO BELONG The Gita highlights. “For the soul there is never birth nor death.Beautifully explained in ” A cloud never dies” teachings by Zen Master Thich Nhat Hanh. “Just as a cloud turns into rain, snow, or mist rather than disappearing, beings continue in new forms, meaning energy and love are never lost, only changed.“
LOVE LANGUAGE sweeps forgotten dust from my recovery, inner sanctuary, pilgrim’s soul. The soul’s love of love is eternal. A wave is not separate from the ocean. A wave is the ocean. Love is not separate from love. Love is an endless ocean of existence.

Buddhist Caves.
Ellora, India.
VIBRATIONAL LIVING is learning from the past, with grace, spiritual elegance, resilient dignity and naturally abiding patience. Being present. Being still. Listen to the silence as the external and inner world harmoniously connect. Liberation from longing. Heightened awareness of being aware.
ACCELERATE SHIFTS IN CONSCIOUSNESS by being in awe of this magnificently divine life. Trusting in intuitively knowing the past, the present and the future. Accountability. Authenticity. Reciprocity. Restorative stillness.
I have learned to love the hurt, until the hurt became love. I was told by a longtime friend in recovery at my first A.A. & Al-Anon (Double Winners) I would learn to listen, listen to learn and heal my life. The universal recovery is massive, millions of like-minded people whose courage to change is inspired and empowered me at the very beginning of my recovery.
LIKEMINDED RECOVERY ADVOCATES Uphold individual, community and universal anonymity – the spiritual foundation of ALL steps fellowships. Whereas in the A.I. addicted world, anyone not committed to holistic sobriety, doing the work, healing relational conflicts will remain in bondage to their drug(s) of choice. Moreover, they will never understand the challenges, courage and commitment someone in longterm recovery.
But that shadow has been serving you!
What hurts you, blesses you.
Darkness is your candle.
Your boundaries are your quest.
You must have shadow and light source both.
Listen, and lay your head under the tree of awe. RUMI
LIVING WHILST DYING addiction is self harm. Pain & suffering. I did to myself what I would not let anyone do to me. Addiction is progressive. Inconvenient consequences. Constant cravings. Compulsivity. Intrigue. Intensity. Suicidal ideation. Shame spirals. Ruptured relationships. Self-abandonment. Blackouts. Betrayal. Chaos. Madness. Suppressed shock waves. Behind the mask: an abject fear of living and dying.
PROTAGONIST & ANTAGONIST The second half of my life, in longterm recovery is a boldly, intentional, curated spiritual practice. Curiosity, wisdom and wonder. A radically changed landscape before recovery, mired by betrayal, self-abandonment, compulsivity, intrigue and intensity. Since that moment of surrender, I continue to existentially thrive. Present moment leaps of faith, trusting in the process, never doubting the efficacy of restorative energy to heal my soul.
PATHWAYS TO PEACE OF MIND is constant awareness of the subtle shifts in consciousness causes and effects. In between stimulus and response the limbic system control mechanisms: the pre-verbal amygdala, the data enriched hippocampus prompt mood regulation, emotionality, congruence and motivation.
ACCEPTANCE is unconditional non-resistance. Accepting unfolding drama and or dharma. Pausing with poise, purpose and patience.
NEGATIVITY is passive judgemental opinions. The shadow’s disruptive inner critic reactive stance talks at and over others attempts to openly, honestly communicating their truth.
OVER-IDENTIFICATION comparing an others’ persona/worldview from a feeling-less-than stance satiating low-esteem spirals.

MASTERSTROKE OF SILENCE: every day I prayed to stop the insanity of obsessively thinking about how I was going to avoid the scrutiny of my then partner the progressiveness of needing vodka, valium and cocaine to function. Denial of progressive avoidant behaviours demands energy. The 12th October 1988. My 1st day of sobriety. I came to. One rarely “wakes-up” from sleepless, dark nights of the soul.
HOPELESS & HELPLESS Alone, anxious and ill a desperation unlike any other, a moment of clarity. I had to get help. What seemed like a relief, took me to the admissions clinic at Payne Whitney psychiatric hospital.
FOREVER JUNG The admitting psychiatrist’s intervention saved my life. She shared with me, Dr. Jung’s belief “aniritus contra spiritum/spirit against spirit” a spiritual awakening/ is essential for the helpless and hopeless alcoholic to end the suffering of an addiction sanskara.
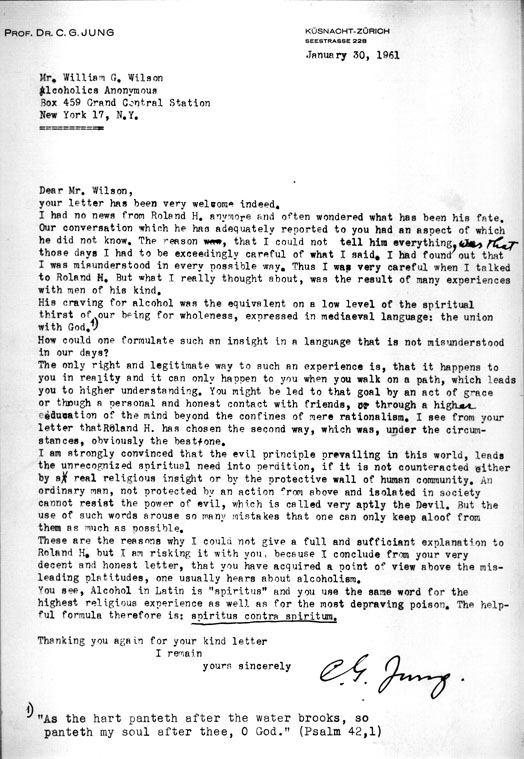
Summoning up courage, I sincerely thanked her. Walking slowly through the hospital gardens, I began to reflect on the previous evening, the insanity of drinking and drugging. Countless blackouts. I felt powerless to stop but hopeful I had endured my last spiral into hell.
INTERVENTION an inner voice silenced by substance abuse suspended reality log enough for me listen: “addiction is not going to kill you, before death comes, you will lose your mind.”For the first time, in a long time, in that moment I felt albeit calmness and clarity. I had experienced a profound spiritual awakening from the relentless, repetitive, long days and darks nights of the soul.
RECOVERY MOVEMENT 12step fellowships meetings at Jan Hus Church @ East 74th Street. Many small steps requiring courage to cross the thresh-hold of the meeting, room. Every step I had taken that memorable day, became the path to lasting recovery. A heartfelt surrender. I came home.
FIRST STEPS 12th October, 1988 was my first day sober. My breath in sync with my heart beats. I crossed the thresh hold, into the universal recovery 12step room moments before the meeting started. Someone from the meeting hugged me and said: “Let us love until you can love yourself.”
1-1 PSYCHOTHERAPY I became willing to change. With patience, and persistence, I am increasingly comfortable with uncertainty. Cues and clues of the past in the present. Therapeutic processes of releasing physic energy/blocks/impasses. Holistic healing from childhood complex trauma, self-abandonment, obsessive thinking, compulsive spirals, patterns and themes.
TRUSTING IN THE PROCESS was initially a great challenge. Freedom from obsessive thinking needing certainty had caused pain and suffering. Learning how to live sober takes practice, and permission. Acceptance requires soul-searching courage.
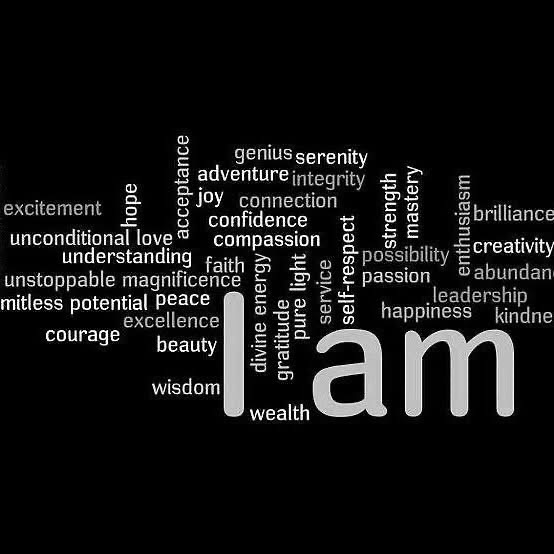
No longer am I defined by complex trauma reactive behaviours. I walk in peace. I am at peace. Present moment leaps of faith, trusting in the process, never doubting the efficacy of restorative energy to heal my soul.
Willingness to access the integrity of recovery’s universal community. A.A. & Al-Anon family meetings/12step fellowship, sponsorship, traditions, and concepts.
NON-JUDGEMENTAL social connections, community and fellowship continues to contribute to 12step longterm recovery pathways: individually and collectively.
BALANCE honesty, tolerance, unselfishness, peace of mind. Self-regulating engenders equanimity. Relieving the bondage of self-obsession.
ADDICTION AWARENESS for 37 years of continuing sobriety I have evolved, and matured. In the immediacy of daily life I am content. Upon awakening I feel gratitude for the dawning of each, new day. I love my thoughts, between stimulus and response bardo/states of mind.
AWAKENINGS AWARENESS Since that moment of surrender, I continue to existentially thrive. Present moment leaps of faith, trusting in the process, never doubting the efficacy of restorative energy to heal my soul, informed by integrating the 12 Step Principles, Traditions, Concepts and Philosophy with contemporary and ancient traditions of Mythology, Psychology and Spirituality.
There are as many definitions of spiritual awakening as there are people who have them. But certainly each genuine one has something in common with all the others. And these things which they have in common are not too hard to understand.
SANSKARIC RELEASING dissolving an addictive (sanskara) impressions is piercing the veil of illusion to awaken the soul, restore consciousness, truth and trust.
Meher Baba Journal vol. 4, No. 7: “the illusion of being finite by (1) liberating itself from the bondage of the sanskaras, and (2) knowing itself to be different from its bodies (gross, subtle and mental). It thus annihilates the false ego (i.e., the illusion that ‘I am the gross body; I am the subtle body or I am the mental body’). While the soul thus frees itself from its illusion, it still retains “full consciousness”, which now results in self-knowledge and realisation of the Truth. Escaping through the cosmic illusion and realising, with full consciousness, its identity with the Infinite Over-soul is the goal of the long journey of the soul.”
UNIVERSAL ABIDING Intuitively solidifying consciousness states of mind, connections and community. Humility centric. Awareness. Cycles of cycles. I incarnated knowing there was God. My earliest innocent archetypal childhood memories of an evolving wild imagination, lucid dreams is a continuing identification with a divine human purpose.
Life is staggeringly surprising. Constantly changing. Our magnificent, limitless universe is beautifully reflected in early an morning dew drop…before the drop becomes the sky in all my tomorrows.
My days flow with life, in alignment, in harmony, love and peace in very breath
I made a commitment to myself in the early recovery days, to seek, to study, meditation, prayer, philosophy, mythology, psychology, and spirituality from wisdom teachers in the art of conscious connection with all that is.
FULL CIRCLE: For four decades, I have worked in both the voluntary and private sectors of universal healthcare in the roles of a volunteer, clinician, psychotherapist, educator, broadcaster, author, writer and end of life companion. In England, Australia, America and India.
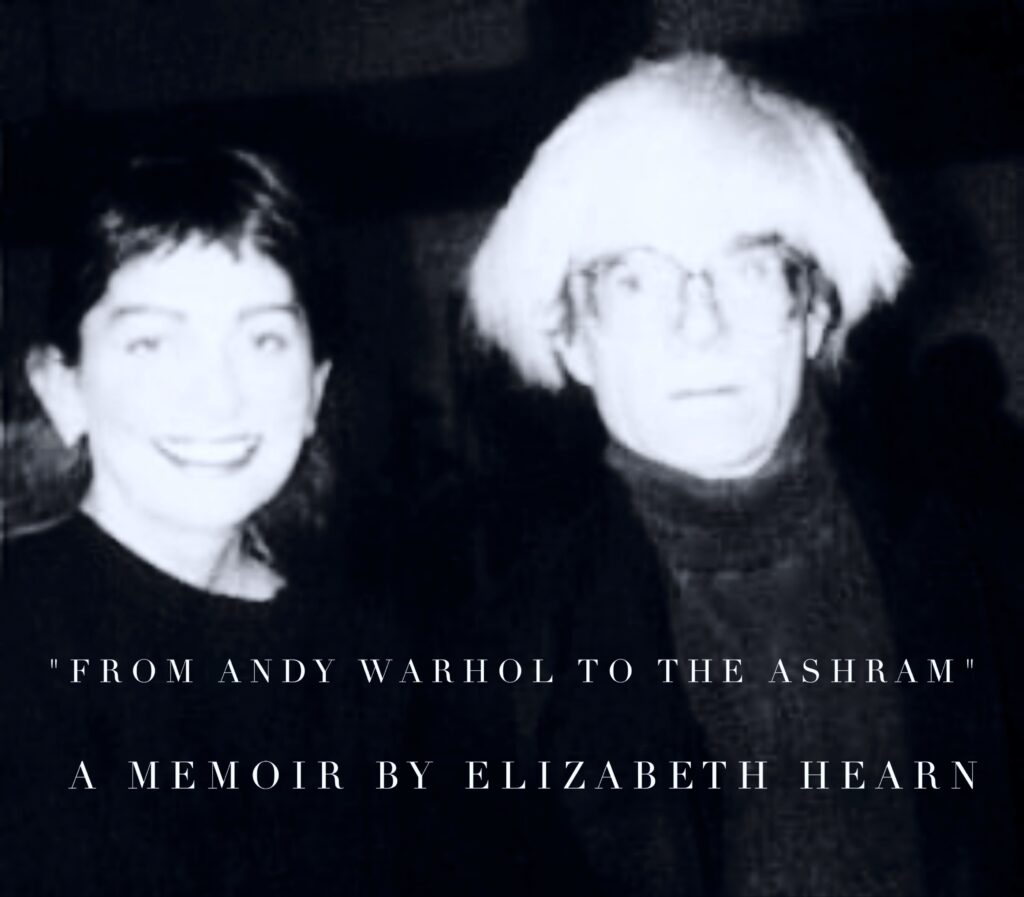
SEVÁ practices began with volunteering alongside my mother, circa 1970’s. Circa 1980’s in the NYC recovery community and fundraising and companions @ Marianne Williamson’s “Manhattan Centre for Living & Dying.” A safe haven for people suffering with AIDS/HIV. Marianne’s selfless dedication to healthcare initiatives remains one of the most humbling, homages to humanity. It was the best of times; joining “A Course of Miracles” Marianne Williamson’s study group circa 1989. In addition to volunteering and fundraising when Marianne founded the “Manhattan Centre for Living & Dying.” A safe haven for people suffering with AIDS/HIV.
Marianne’s selfless dedication to healthcare initiatives remains one of the most humbling, homages to humanity. Sevá – being of service specifically to ease pain and suffering one person at a time.
TRANSCENDENT TIMELESSNESS: the present moment is my primary focus. Strength in stillness presence is synonymous with transcendent experiences. Awareness. Intuitive mind. Existential alignment. Authentic awareness.

PRANAYAMA karma/calmness and composure. Oftentimes when I am experiencing in the moment fear and self-doubt, I close my eyes and breathe. Visualise following the gentle release of the breath. Oh joy, my constant companion. Opening my heart to love to graceful acceptance.
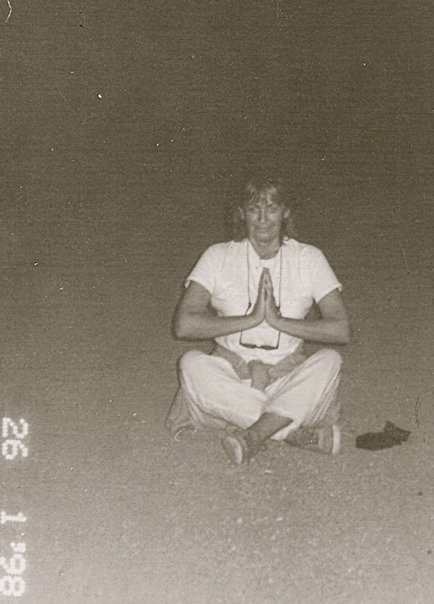
A CONTINUUM OF SOBRIETY is living in this moment absolutely beautiful moment. Stillness. Peace. Comfort. Everything and or nothingness, all at once. Meditative meditation minimalism. Breathwork. All the while experiencing the breath as love. I have come home to myself, with God’s grace, with tenderness, and great love.
LOVE ALONE PREVAILS. Love brings wholeness and transformation in the everydayness of life. Reciprocity. Renewal. Universal recovery.Since that moment of surrender, I continue to existentially thrive. Present moment leaps of faith, trusting in the process, never doubting the efficacy of restorative energy to heal my soul. Compassion is an invitation to consciousness. Cultivating seeds of wholeness in one’s fertile imagination.
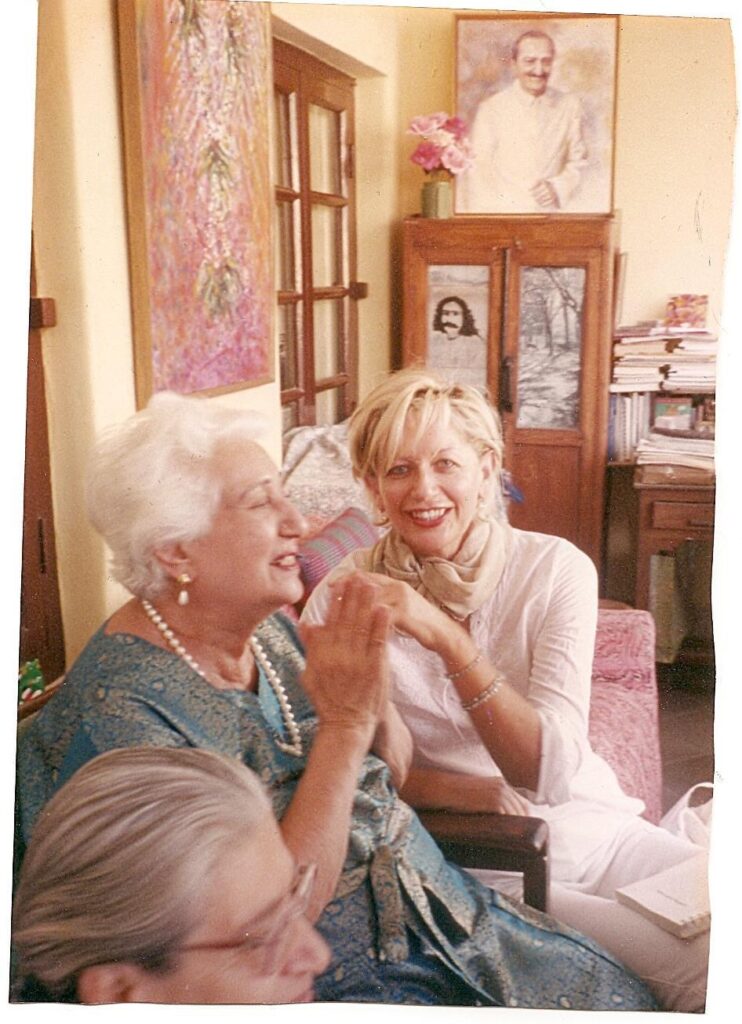
An impactful event so unsettled me I felt called to live in a rural village established in 1939 by Meher Baba whose message to the world: “I have not come to teach but to awaken.” emphasizes that true divinity is realized through love, selflessness, and abandoning the ego. He advocated for experiencing the oneness of all life to overcome illusion, fear, and materialism.
The Goal is Love: The highest path is to love God with all one’s heart, which naturally leads to realizing one’s own divine nature.
The Illusion of Separation: He taught that God is in everyone and everything. Meaning all souls are fundamentally one.
Awakening over Doctrine: Rather than establishing new religions, he came to re-awaken humanity to the truths taught by previous avatars like Christ, Buddha, and Krishna.
Balance of Life: He advocated for blending “realistic West with the idealistic East,” meaning a balance of material, intellectual advancement with spiritual, heartfelt realization.
Actionable Advice: He urged followers to practice honesty, avoid hypocrisy, and serve others to transcend the ego.
Meher Baba also emphasized that the material world is essentially a shadow of reality, and that real, lasting peace comes from within.

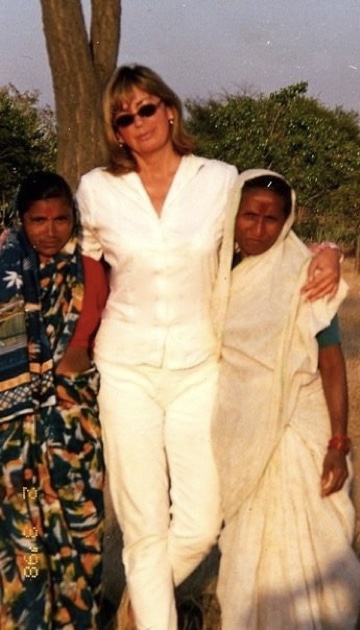
TIMELESS INDIAN TIMES I lived nearby Meher Baba’s Ashram in 1998-1999 at a friend’s fabulous house. Days would pass without speaking to anyone. In the silence was love beginning with myself. I had opened my heart to love. Everything I was experiencing- alone, sadness, longings, I named love.
SACRED LAND Volunteering at the free dispensary/hospital. The beautifully situated school. In the immediacy of pilgrim daily life, much love, happiness and harmony. A homage to being of service. A continuum of awakenings.
Waking up in India’s early morning is a celebration of life: Fabulous sunrises. Magnificent conference of the birds singing to God as I walk where Baba had walked many times up the hill to morning prayers/puja.
Solitary walks, alongside robust coriander fields. I felt deeply connected to the land, the people and way of life, The past in the present. An ancient sense of knowing God of my understanding was awakened, engendering intimate connections with people I love.
RELEASING ENERGY BLOCKS Beautiful emotional energy. Wisdom sparks spontaneously appeared in conversations, or lovely walks and talks. Life was a daily pilgrimage, all about connections and communion with the universe.
GLIMMERS OF ILLUMINATION : symbolic signals from God, powerfully oftentimes, tender prompts healing trace triggers of my soul’s individual signature from the longest dark nights of the soul.
PAST IN THE PRESENT spiritual recovery is in derivatives of BARDO teachings Ancient and contemporary Eastern philosophy, mythology, psychology, theology and spirituality. BARDO’s “between states/stimulus and response.”
SELF CARE: I have healed my soul’s individual, ancestral and collective trauma, complex dimensions of family systems from the pathos of addiction, anxiety, depression, grief and loss.
Shame, trauma, self-abandonment, shame, grief, and self-hatred, heals into mindsets where hope and love connect. Breakthroughs became my best moments in therapy. My personal foundation for healing my soul is in becoming teachable.
PILGRIM LIFE in 2020 a universal new order of life necessitated by COVID guidelines for personal safety ushered in new self-care habits. I adjusted to 12 step zoom meetings, the new normal way to connect with my recovery community.
The timing was perfect during universal lockdown to study, reflect and learn. I trained in lucid dreaming, and BARDO insights both practical and tactical relative truths with the wondrous Andrew Holecek. In addition to silent skies, streets and the park the serenity of being at home, cooking, reading, walks and talks with my husband, meditating, walking barefoot in the garden, listening to birdsong was simpler, kinder and connected to all that is without the need to be anywhere, do anything that I did not want to soon became a way of life that continues, every day in every way.
SEEKING MEANING in my early 20’s my younger, innocent self struggled to understand complex ancient traditions, principles and philosophy of “Upanishads, The Tibetan Book of Living and Dying and the Bhagavad Gita ” collective themes “dying before you die” philosophy.
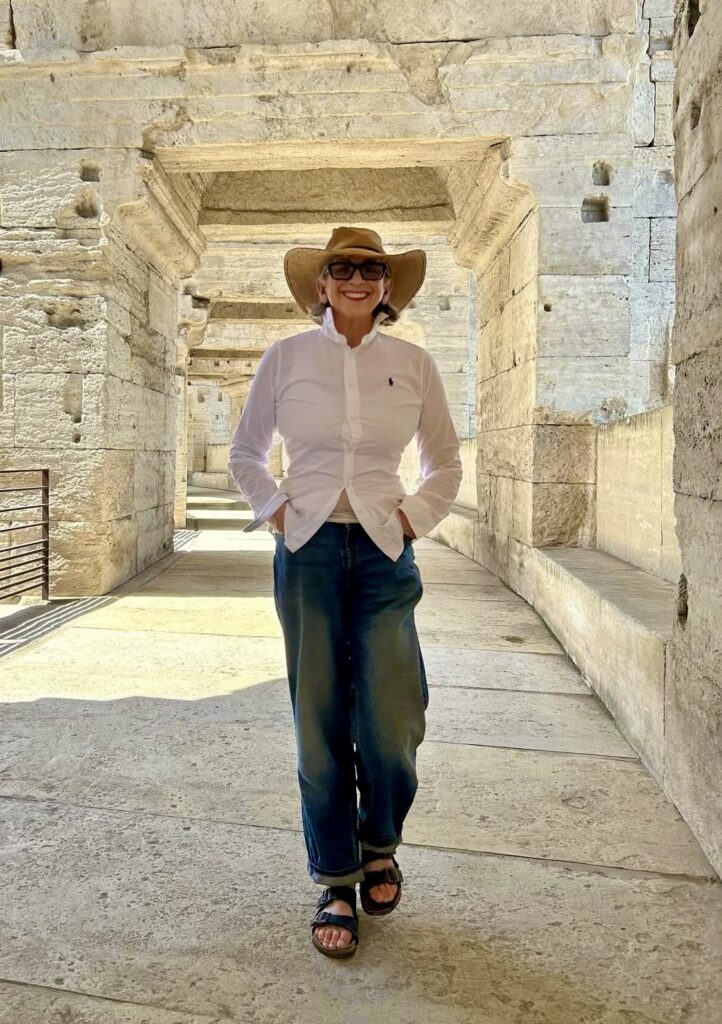
In my 70’s, walking around this magnificent earth, 50 years into my daily spiritual practice, in tandem with pilgrimages/travelling to sacred lands, reading, training, studying and deep learning I am comfortable with the practice of “dying before I die.” Much joy and happiness.
ANCESTRAL LEGACIES How we chose to evolve from ancestral, cultural, gender, and societal constructs – nature versus nurture/learned behavious upon our relationship with God, Buddha, higher power etc of our understanding, a lifetime of constructs about life and death is either limitless or limited…It is my understanding of living and dying that I am not this body. My soul is eternal.
LOVE LOSS & GRIEF is a heartbreaking process. A lifetime of core beliefs about themes of living and dying were ripe for a transcendent journey inwards when my father died in 1997.
We shared a love of the ocean, of beauty, healing the soul despite his confrontational communication style he challenged me to be curious, to be compassionate, to be victorious.
His “afterlife” spirit is a constant companion. His “dying before you die| lesson to me occurred when he was admitted to Intensive Care 10, 000 miles aways, from my home in London. We were physically but not spiritually separated by time and distance.
It was all I could do to connect with him in spirit. I asked my mother to quietly tell him I loved him unconditionally. During a long-distance consult call I discussed my father’s end of life wishes with his doctor, my mother and siblings. Intuitively, I knew he was ready to go, while in a coma he was moving through the various stages of Bardo.
My family despite our differences, respect our families highly individual, different beliefs around living and dying. We prayed my father’s last exhale moment would signal an end to his suffering.
And so it goes, his leaving the body took a few days whilst at he momentarily “appeared” at night just before I fell asleep, his form, shadow-like translucent, appeared in the silence, and stillness of the night my father “spoke” of his love for me. Timelessness. A Gestalt closing the loop of a thousand unanswered questions dissolving in the silence.

OCEANS OF LOVE I would read this beautiful poem before I undertook the process of working through the 12steps to ground my sense of integrity, willingness, hope and forgiveness“ making amends to family, friends and peers I had hurt, betrayed and blamed in blackout, hungover, and always angry remember bowing at their feet, extending gratitude for giving me life, and asked for their forgiveness for rejecting their love. Afterwards, I experienced an energetic, oceanic, love surge.
“It is said that before entering the sea
A river trembles with fear.
She looks back at the path she has travelled,
from the peaks of the mountains, the long winding road crossing forests and villages.
And in front of her, she sees an ocean so vast, that to enter there seems nothing more than to disappear forever.
But there is no other way.
The river can not go back.
Nobody can go back.
To go back is impossible in existence.
The river needs to take the risk of entering the ocean because only then will fear disappear because that’s where the river will know it’s not about disappearing into the ocean, but of becoming the ocean.”
~ Khalil Gibran
Learning to love the hurt until it becomes love, from this life to the next with so much love, compassion and connection.
NON ATTACHMENT I was a surfer for many years. I adored listening to the sound of waves whilst sharing mixed metaphors with other surfers usually about the meaning of life.
CHANGE IS CONSTANT Sometimes the power of waves energetically rushes to the shore, other times it is an elegantly quiet series of waves protectively easing towards the shore. Everything passes. Everything is connected, we are ONE. We are the ocean of love.
LOVE ALONE PREVAILS: A deep bow to my husband. I adore falling asleep to the rhythmic sounds of his breathing. His habitual, light snoring signals he is transcending into dreamtime.
In the still of the night, I feel loved, calm, safe and happy with this handsome, spiritually elegant soul. We reflect the many ways of loving oneself, one another, one’s close family and friends. Co-existing with self-compassion, creative expression and companionship. His quiet soul. His smiling dimples-on-display humour. Collectively we aim to be in flow with being loved.
My love of philosophy, mythology formulates into a humanistic, archetypal, symbolic perspective, inspired/intuitive deepening awareness. Mindfully manifesting strength in stillness.
DYSREGULATION is a critical mass mental health phenomena. The un-reality is that its all too easy to project blame onot others. Unbridled pursuit of power, money, celebrity corrupts to the core, the soul.
UNCOMFORTABLE WITH UNCERTAINTY Considering, the definition of insanity is repeating the same behaviour but expecting a different outcome. The illusion of needing to know, satiates the despair of fear, doubt and uncertainty.
AUTHENTICIY The reality of knowing why we need to do something to take away feelings of anxiety and The action involved in doing this differently thereby making healthier choices requires awareness, courage and commitment.
COME CLOSE – GO AWAY avoidant personality. An inability to sustain intimate, closeness and connection in relationships. Emotionally, spiritually, psychologically and physically barricaded.
SUPER EGO entitlement agenda. Arrogant. Coercive control. Addicted to power. Money. Fame Scrutiny avoidant.
MAGICAL THINKING is an addiction to fantasy. Whereas reality challenges us to choose between fake or reality prompts for conscious awareness require awareness, courage and commitment.
SUPPRESSED ENERGY arrested development. Dysregulation. Many dark nights of the soul – compounded by abject loneliness. Inconsistent nability to self care.
FELLOWSHIP LEGACIES A.A. CO- FOUNDER OF Bill Wilson had his first drink while in the Army during World War I. “I had found the elixir of life” he recalled, and he soon began to drink heavily. After the war, he married Lois Burnham in 1918 and enjoyed great success trading stocks on Wall Street. He lost all of his money in the stock market crash of 1929, but he continued to trade stocks and managed to earn a modest living. However, his heavy drinking continued to get worse, and it slowly took its toll.
Eventually alcohol completely took over his life and by 1933, he had hit bottom. Bill and Lois were living in her parent’s home in Brooklyn. Lois was working in a department store, while Bill spent his days and nights in a near-constant alcoholic stupor.
In 1934, he was visited by an old drinking buddy who had managed to stop drinking and stay sober. He shared his secret with Bill; a belief that God would help him overcome his addiction to alcohol. When Bill said he was not a member of any organized religion his buddy said, “Why don’t you choose your own conception of God?” Bill understood that “it was only a matter of being willing to believe in a power greater than myself.”
As Bill later recounted, “God had done for him what he could not do for himself.” Bill Wilson had a spiritual awakening and his belief in a higher power and the realization that he couldn’t do it alone would help him to conquer his addiction. Determined to get better, he checked into a hospital and underwent the state-of-the-art treatment at that time for alcoholics “the barbiturate and belladonna cure, also known as “purge and puke.”
“While I lay in the hospital, the thought came that there were thousands of hopeless alcoholics who might be glad to have what had been so freely given me. Perhaps I could help some of them. They in turn might work with others.” He then came to understand how helping others would be essential to his recovery.
After his release, he managed to stay sober but returned to the hospital frequently to help other alcoholics undergoing detox. It was during this time that he faced his moment of truth at the Mayflower Hotel and began his association with Dr. Bob Smith. Wilson and Smith helped each other and then reached out to other alcoholics. Soon they began to hold meetings for recovering alcoholics so that they could support their group and welcome others who were looking for help.
My dear friend Lorna Kelly would often begin her share at a 12 step meeting with the question: “What if Bill Wilson had a “good day” in Akron…?” He was a few months sober, on a business trip to Akron, Ohio. The business venture meeting did not go according to plan. Bill, feeling rejected, faced a lonely weekend in the Mayflower Hotel, Akron.
The potential to relapse, all too easy to walk into the cosy hotel bar, instead Bill remembered his wife Lois’s words: Bill had remained sober by helping another alcoholic.
He looked through the hotel church directory and found a strange name which caught his attention – Reverend Walter Tunks (Tunks is a word used in Bill’s home state of Vermont).
Bill called Rev. Tunks and received a list of people to call. After many failed calls he finally made contact with Henrietta Seiberling of the powerful family which owned the Goodyear tyre company.
Henrietta Seiberling responds to Bill’s call and immediately thinks of her Oxford Group friends (Dr. Bob Smith and his wife Anne). The Oxford Group has prayed for help for Dr. Bob and Henrietta sees Bill’s call as literally an answer to these prayers.
It’s the day before Mothers’ Day and Dr. Bob has come home with a plant for Anne. Both the plant and Dr. Bob are ‘potted’. Bill’s visit is delayed until the Sunday (Mothers’ Day) so that Dr. Bob can sober up to meet with Bill.
RECOVERY PATHWAY TO FREEDOM
Maybe there are as many definitions of spiritual awakening as there are people who have had them. When an addict has a spiritual awakening, they are willing to change.
They has been granted a gift which amounts to a new state of consciousness and being. The way forward. There is hope. something to be endured or mastered. In a very real sense transformation happens. A source of strength.
They find them self in possession of a degree of honesty, tolerance, unselfishness, peace of mind, and love. Self-regulating engenders equanimity. Relieving the bondage of self-obsession.
I love my life in recovery. Nothing happens a moment before it is meant to. the courage to change is infinite. I hope you find this to be true for you.
Saversham.